What is a Scenario Model?
The scenario model used for this analysis of potential future states for various payer and reimbursement models is derived from The Art of the Longview by Peter Schwartz. The scenario model is:
- A method for investigating important decisions.
- Designed to invent and then consider equally plausible futures.
- Prepares an organization for any plausible future.
- Investigations are based on “critical uncertainties” – pivotal elements that act unpredictably.
- The scenario process provides a context for thinking clearly about the impossibly complex array of factors that affect any decision.
The Relevance of a Scenario Model for the Transforming US Healthcare Market
US healthcare organizations need to be able to be able to evaluate strategic plans for all plausible futures that may exist as healthcare insurance and reimbursement models transform from fee for service to fee for value, or capitated environments. Many health system CEOs are concerned that the US will move to a “Medicare for All” (M4A) environment more quickly than they can position their organizations to be successful in such an environment. As we watch the market it is apparent that M4A is only one plausible future scenario. Current market drivers impacting strategic planning processes are:
- Value-based care models (e.g. MIPS, APMs, bundled payments).
- Employers forcing more healthcare costs on their employees.
- States signaling moves toward single payer models.
- States launching insurance plans to compete with commercial insurance (e.g. Washington state).
- States entering private/public ACO partnerships to control Medicaid costs (e.g. Texas).
- Large companies creating new insurance/care delivery models (e.g. Haven).
Being able to create scenario models for an organization’s market that can identify likely transformations will increase an organization’s success factor for future viability.
Digital Technologies That Will Impact Future Organizational Model Outcomes
As we evaluate a scenario model for future healthcare potentialities, we must also understand that organizational outcomes for successfully transitioning to the future is directly related to how well organizations adopt and implement digital technologies that are needed to support new healthcare delivery and reimbursement models.
- Accurate data analytics of healthcare delivery services and populations to better manage care deliver through process improvement.
- Social Determinants of Health (SDOH) applications to improve care quality and access to care.
- Advancing AI capabilities applied to data analytics (e.g. real-time monitoring/surveillance of patient data and operational data) for better identification of patient(s) at risk.
- Patient engagement bots (e.g. mobile applications that interact with patients to provide appropriate care guidance).
- Digital assistant solutions (voice recognition and AI) for capturing patient information/data for EHR documentation, and more efficiently “hands free” navigation of the EHR for the clinicians.
- FHIR standard APIs to drive effective interoperability between systems that hold a patient’s data
- Hybrid RCM applications that support both FFS and FFV in the hybrid reimbursement world.
- Sophisticated contract management and cost accounting systems to better manage value-based care contracts.
- Compelling healthcare organization web sites that encourage patient interactions with the healthcare system (e.g. personal health record access and interactions, scheduling of patient services, ability to pay bills, seamless specialist services, ability to text or email with care providers).
Critical Uncertainties
Critical uncertainties are unstable or unpredictable, such as future healthcare reimbursement models, future payer/insurance models, government regulations, or new technologies or products. A critical uncertainty is an uncertainty that's key to evaluating plausible strategies. Representative critical uncertainties that were evaluated for creating the scenario model were:
- How will healthcare access, cost, and quality be improved?
- How will the current “Medical Industrial Complex” be disrupted (e.g. payers, providers, pharma, PBMs, commercial laboratories, supply chain organizations)?
- What will be the role of current payers in a future healthcare model?
- What payment models will predominate in the future?
- How will healthcare reimbursement models emerge for the general population (e.g. at the state level or at the federal level)?
- Will there be a patchwork of healthcare reimbursement models across the country?
- To create the scenario model for evaluating future healthcare environments the following critical uncertainties were selected:
- The reimbursement model uncertainty – capitated versus value-base care; as we slowly move beyond fee for service, providers need to prepare for lower reimbursements. Capitated as represented by Medicare for All (M4A), and value-based care that provides the ability to receive higher reimbursements for providing high quality care with top outcomes.
- The payer landscape model uncertainty – single payer versus multi-payer. M4A will move the country to a single payer format like the UK and Canada. The multi-payer model represents a less disruptive approach for controlling healthcare costs but may force commercial payers to become competitive with government sponsored payer plans, or to create partnerships that deliver lower costs with higher care quality and outcomes.
These uncertainties represent top of mind discussions for most healthcare executive teams and boards as they are exposed to evolving insurance and reimbursement models in their markets.
The Scenario Model Quadrant
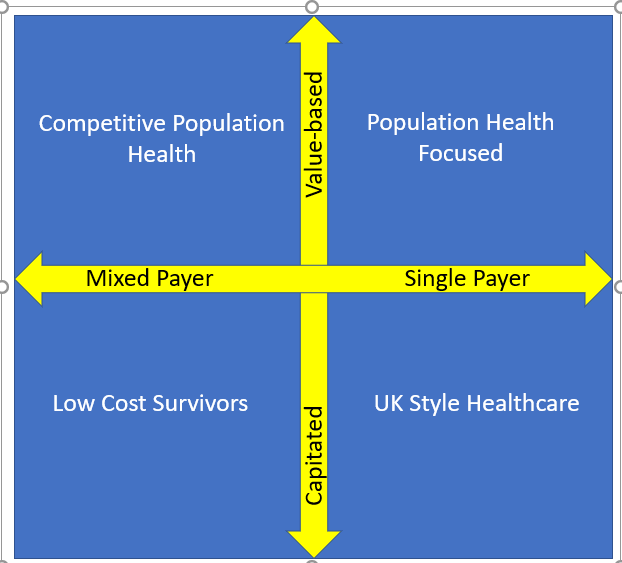
The critical uncertainties selected resulted in quadrant axes representing potential insurance (single/multi-payer) and reimbursement (capitated/value-based) environments. Using these axes, four quadrants were developed as depicted in Diagram 1.
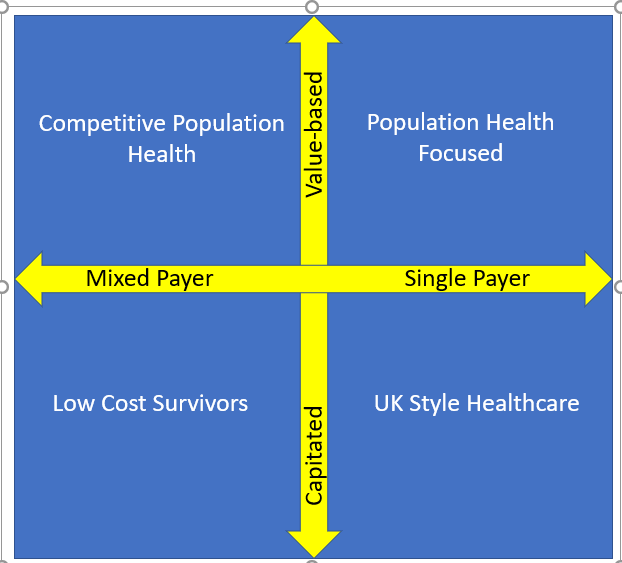
Diagram 1
Each quadrant requires organizations to modify existing and/or develop new care delivery processes to survive the healthcare transformation that is upon us. As we review each quadrant in subsequent articles, we will identify organizational processes that will need to be examined to create effective strategies for healthcare markets. We will also review events (media headlines) that can be used to assess which quadrant best represents an organization’s market. Once a quadrant is identified, the healthcare system can begin to implement strategies to position itself for a successful transition to future viability.
Start Now!
No matter which quadrant a healthcare organization identifies as the most probable future state, they should begin to implement processes that will be applicable to any quadrant. These activities include:
- Initiate activity-based costing for the top 10 organization services by reimbursement amount and/or by volume.
- Use lean or continuous quality improvement projects to drive cost, workflow efficiency, and quality improvements for top services being analyzed.
- Evaluate staffing license requirements for services being analyzed; can lower cost staff provide services without impacting care quality or patient safety?
- Evaluate digital technologies for improving service costs and outcomes with a focus on mobility solutions that support all modalities of care.
- Drive the highest level possible for interoperability with other providers who care for patients in your market.
- Analyze supply costs and services to drive down costs and improve supplier performance for analyzed services.
- Improve patient engagement services using bots for scheduling services, accessing patient health records, ordering medications, addressing FAQs, and paying bills.
Lastly, continue to monitor new insurance and reimbursement models that are emerging in your markets. They may not succeed in the long run, but they will test an organization’s operational flexibility for remaining viable.